 Chronic pain clearly isn’t just in your head, but according to a new study, psychiatric disorders or mental health issues may lead to an uptick in perceived conditions.
Chronic pain clearly isn’t just in your head, but according to a new study, psychiatric disorders or mental health issues may lead to an uptick in perceived conditions.
For their study, researchers in Brazil examined more than 200 individuals who believed they were suffering from Gastroesophageal Reflux Disease, or GERD. GERD is very similar to chronic acid reflux, where patients suffer a burning sensation when stomach acid makes its way back through the esophageal sphincter and into their lower esophagus. All individuals received a comprehensive medical exam and were asked to complete a 14-question survey that analyzed their mental health for signs of depression or anxiety.
Anxiety, Depression and Pain Perception
After completing the medical exams and reviewing the survey results, researchers came to an interesting conclusion. Nearly half of the patients who reported having anxiety or depression had normal acidic pH values in their esophagus, suggesting that they most like did not have GERD. However, this doesn’t mean that patients are crying wolf about their perceived symptoms.
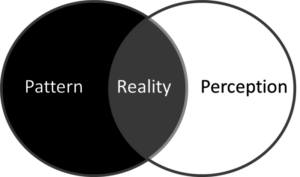
“Patients with anxiety and depression or other mental health issues display a ‘hypervigilance’ or ‘hypersensitivity’ to pain sensations,” said lead researcher Dr. Fernando Herbella.
Moreover, researchers uncovered an inverse relationship between anxiety levels and esophageal pH; the more anxious a patient was, the less damage they had in their esophageal lining.
Dr. Vic Velanovich, a co-author on the study, offered a neurological explanation for the link between mental disorders and pain perception.
“It’s called the ‘pain modulation network.’ Pain is converted to electrical signals that travel to the brain. It’s interpreted there by the frontal cortex. So anything happening in the frontal cortex, including mental disorders, makes pain perception worse.”
The subject matter is near and dear to Dr. Velanovich, who worked on a similar study back in 2011. In that study, Dr. Velanovich studied patient satisfaction after GERD surgery. Most notably, surgery satisfied 93.5 percent of patients without psychiatric disorders, but only 11.1 percent of patients with a disorder.
“It was a classic ‘nocebo’ effect,” Velanovich says. “For both groups of patients the GERD pain was greatly relieved. But only anxious patients found the aftereffects of the surgery intolerable. Which tells me that there’s something else going on.”
These two studies highlight the importance of getting a comprehensive medical diagnosis by a pain care provider who knows all the signs to watch for. Unless all the underlying issues are treated, you’re not going to acheive full relief. To learn more about the association between mental health and the perception of chronic pain, or to talk to a specialist about another issue, reach out to Dr. Cohn today.
