 If you’re a regular reader of our blog, you know our views on opioids for pain management. Used correctly, opioids can be a wonderful compliment to a chronic pain management program, but their use can also cause some health issues even when carefully taken. According to a new study, not only can starting an opioid regimen be potentially hazardous to your health, so too can stopping opioid use. This doesn’t mean that you should plan to take opioids indefinitely, but it speaks to the importance of working with a pain management provider when starting and stopping an opioid regimen.
If you’re a regular reader of our blog, you know our views on opioids for pain management. Used correctly, opioids can be a wonderful compliment to a chronic pain management program, but their use can also cause some health issues even when carefully taken. According to a new study, not only can starting an opioid regimen be potentially hazardous to your health, so too can stopping opioid use. This doesn’t mean that you should plan to take opioids indefinitely, but it speaks to the importance of working with a pain management provider when starting and stopping an opioid regimen.
According to a recent study published in the journal PLOS Medicine, stopping a prescription opioid regimen can actually increase a person’s risk of overdose death. Opioid-related overdoses are a major concern here and in Canada where the study was conducted, and researchers wanted to learn more about the potential impact of discontinuing an opioid treatment plan. You might inherently believe that your risk of overdose falls to zero if you stop taking opioids, and in a perfect world, you’d be right. However, not everyone who stops taking opioids can do so easily, and therein lies the risk of eventual overdose.
Safely Stopping Opioid Use
For the study, researchers reviewed the medical records of more than 14,000 patients in British Columbia who had been on opioid therapy for at least 90 days. After reviewing the records, researchers found that discontinuing opioid therapy for chronic pain was associated with an increased overdose risk for people without an opioid use disorder (OUD). An inverse effect was seen in patients who tapered off of opioid use, as their overall risk of overdose decreased. Researchers concluded that abrupt opioid stoppage could be dangerous, and that patients should work with a provider to taper off of medications so as not to increase their risk of overdose as they seek to end an opioid regimen.
While there were some limitations in the study, including whether or not associated overdoses occurred with prescription medications or those obtained illegally, the general message holds true in that it is extremely important that you work with a physician when working to stop an opioid treatment plan. We understand that you are aware of some of the potential issues associated with opioid use, and we commend you on wanting to curb or eliminate your reliance on these medications. However, there is a right way to go about cutting prescription medications out of your system. Sometimes slow and steady wins the race, and cutting opioids cold turkey could have some unintended withdrawal effects.
If your current medication plan isn’t getting you where you want to be, talk to a doctor about safely adjusting your medication program. We want to help you find the right solution, but finding the right treatment is only part of the battle. You also need to approach the treatment in the right manner, otherwise you may face some unexpected obstacles.
For more information, or for help with a chronic pain condition, reach out to Dr. Cohn and his team today at (952) 738-4580.
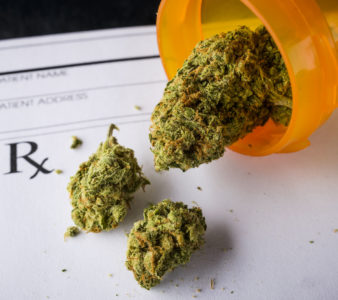 New research has found that nearly one-third of patients with chronic pain report using medical cannabis to manage their pain, with more than half of them decreasing their reliance on other pain medications, like opioids, in the process.
New research has found that nearly one-third of patients with chronic pain report using medical cannabis to manage their pain, with more than half of them decreasing their reliance on other pain medications, like opioids, in the process. A growing number of US adults with chronic pain are pursuing a combination of non-drug and non-opioid approaches to control and treat their condition, which is an encouraging sign.
A growing number of US adults with chronic pain are pursuing a combination of non-drug and non-opioid approaches to control and treat their condition, which is an encouraging sign. Opioids are a hot-button issue in the chronic pain community, and rightfully so. They can absolutely play a vital role in helping someone overcome a chronic pain condition, but they are also much riskier than other treatments that don’t carry a likelihood of overdose and dependency. We’ve seen firsthand how opioids can be a perfect compliment to a chronic pain management program, but we also want to give patients an opportunity to avoid painkillers if they so choose as part of their recovery plan. In today’s blog, we showcase five alternatives to opioids for chronic pain management.
Opioids are a hot-button issue in the chronic pain community, and rightfully so. They can absolutely play a vital role in helping someone overcome a chronic pain condition, but they are also much riskier than other treatments that don’t carry a likelihood of overdose and dependency. We’ve seen firsthand how opioids can be a perfect compliment to a chronic pain management program, but we also want to give patients an opportunity to avoid painkillers if they so choose as part of their recovery plan. In today’s blog, we showcase five alternatives to opioids for chronic pain management.